The purpose of contingency planning is to anticipate a disaster or crisis. A whole range of measures, procedures, tools and coordination mechanisms are put in place. This way, resources (both human and equipment) necessary to manage the situation can be deployed quickly and efficiently. Depending on the nature of the incident, there are several different contingency plans.
- The multi-disciplinary contingency plans are developed by different authorities. These contingency plans are intended for crisis management at a national level. For example, this type of contingency plan was used during the bus disaster in Sierre, the terrorist attacks in Zaventem or the COVID-19 crisis;
- Mono-disciplinary intervention plans: This plan aims to develop the missions per discipline, so a discipline can start independently and act quickly. In addition, an intervention plan makes it possible to collaborate with other disciplines;
- Internal emergency plans: These are plans drawn up at the level of an institution, e.g. a hospital.
To find out more about emergency plans: www.crisiscentrum.be
Below, we will examine the mono-disciplinary intervention plan for medical, sanitary and psychosocial assistance (discipline 2), for which the FPS HFCSE is responsible in an emergency situation.
This intervention plan describes the following missions:
- Initiating the medical chain;
- Administering medical and psychosocial care to victims and people involved in the emergency situation;
- Organising the transportation of victims;
- Taking measures to protect public health.
3 specific sub-plans that were developed as part of the above missions will now be discussed.
|
MEDICAL CARE |
PSYCHOLOGICAL CARE |
PUBLIC HEALTH |
||
|
Medical MIP |
Psychosocial PSIP |
Risks and RDP |
THE MEDICAL CONTINGENCY PLAN (MIP)
The first aid groups (police, ambulance service or fire brigade) on the scene can request the activation of a medical contingency plan (MIP)[1]. Only a few professionals are positioned to activate a MIP, namely:
- the (deputy) director of medical assistance[2];
- the first MUG/SMUR doctor at the scene;
- a federal health inspector;
- an ‘Incident and Crisis Management’ (ICM) expert;
- the (deputy) department head for emergency assistance from the FPS HFCSE.
Ultimately, the emergency centre, which has territorial jurisdiction, will formally declare the MIP.
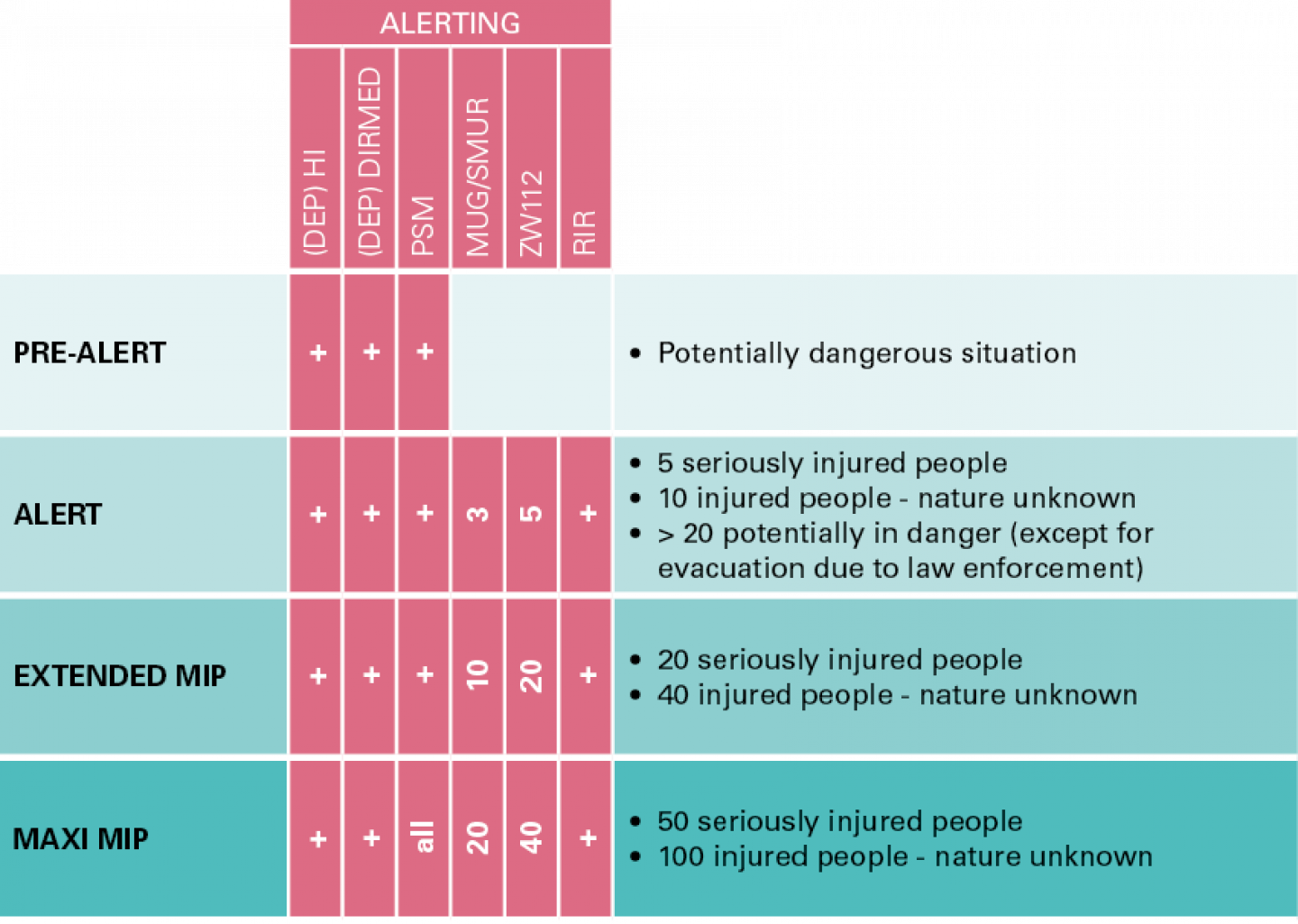
A MIP has different levels, with an increasing deployment of resources depending on the phase the MIP has reached. The (deputy) health inspector ((DEP)HI), (deputy) director of medical assistance ((DEP)DIRMED) and psychosocial manager (PSM) are always called. Depending on the phase, the Medical Emergency Group (MUG/SMUR), ambulances (ZW112) and rapid intervention resources (RIR) are deployed.
The scaling up and down of plans is carried out by the emergency centre on the basis of the information obtained from the people referred to above. When a MIP is scaled up, the affected province can call upon the resources of neighbouring provinces.
The federal Minister of Public Health has an agreement with the Belgian Red Cross to provide support in the event of a (medical) emergency. This includes, among other things, providing for the following:
- Ambulances and paramedics
- Rapid Intervention Resources (RIR) for the establishment of the advanced medical post
- Liaison officers: these are people who establish contact during an emergency and ensure communication between the various partners involved.
- Logistical support (sanitary kits, camp beds, blankets, etc.)
- A roll-out in ‘Emergency Social Intervention’: these are volunteers who provide emergency psychosocial support in large-scale relief operations during disasters or severe cases.
The (deputy) director of medical assistance, the federal health inspectors and the ‘Incident and Crisis Management’ expert coordinate medical assistance during a crisis. When the crisis is of such a magnitude that major socio-economic consequences are feared, the administrative management (mayor, governor) is also called upon.
|
FOR EXAMPLE During a large industrial fire, a toxic cloud moves towards surrounding businesses. At that point, a decision must be made as to whether the factory must be evacuated for health reasons. This decision is made by the director of the operations command post or, in the administrative phase, by the mayor or governor. This decision has financial implications. Compensation may also need to be paid. The various disciplines have an advisory role at the municipal or provincial coordination centre (CC) at that point. |
THE PSYCHOSOCIAL INTERVENTION PLAN (PSIP),
A collective emergency could cause serious psychosocial damage to a large number of people. As a result, there may be a need for adequate assistance for those directly involved and their loved ones. In order to address this need, a Psychosocial Manager (PSM) works alongside the Federal Health Inspector (FHI). The actions within psychosocial support are aimed at stimulating the resilience of those affected and are targeted at both the direct and indirect victims of the emergency situation. The federal government is responsible for psychosocial assistance in the acute phase. The psychosocial assistance in the aftermath is a task for the communities.
The following basic tasks of a psychosocial manager are to be carried out in the acute phase of an emergency situation:
- grouping the uninjured at or in the vicinity of the disaster area;
- transporting the uninjured to a reception centre;
- installing and developing a reception centre (RC) where psychosocial support and information can be provided to those involved;
- installing and developing a Telephone Information Centre (TIC) for those directly affected and their relatives;
- uniform registration: the accurate collection of information about those affected and its safe management;
- processing the data to create victim lists at one central point (Central Information Point – CIP).
|
EXAMPLE During a fire at an assisted living facility, the family needs information about their family member. The PSM concerned will organise an information point at a nearby sports hall. |
To find out more about PSIP: www.health.belgium.be
RISKS AND DEMONSTRATIONS PLAN (RDP)
When a large-scale activity is organised, it may be necessary to provide a medical aid station as a precautionary measure. Using the RDP questionnaire (Risks and Demonstrations Plan), the health inspectors give advice based on a risk analysis. The competent authority (the mayor or governor concerned) is advised on the necessary medical resources.
To find out more about RDP: besafe.jdbi.eu
[1]The structure of the MIP is defined in a ministerial circular.
[2]This is a position in the MIP where a physician is in operational charge of all medical, sanitary, and psychosocial support services at the site. This doctor works under the administrative authority of the federal health inspector.
