- Details
In each COVID-19 wave, we notice a marked peak in the number of infections and in the positivity ratio[1].
The highest number of infections were detected in the 5th wave with a peak of more than 50,000 infections per day on average.
DAILY NUMBER OF NEW COVID-19 INFECTIONS AND TESTS TAKEN [2]
The number of people tested has shown an upward trend since the beginning of the pandemic, with an initial peak of over 65,000 tests per day on average during the second wave. This equates to a tripling of the number of tests per day compared to the first wave. Fewer tests were being taken at that time because testing capacity was limited. Consequently, fewer infections were detected. The testing strategy was altered several times throughout the pandemic and this affected the number of tests taken. For example, between 21/10/2020 and 22/11/2020, only persons with symptoms were tested and no tests were taken for persons with high-risk contact; from 2/2/2021, children over 6 years of age were also being tested. During the fourth and fifth waves, testing was at maximum capacity and an average of 120,000 tests were taken per day.
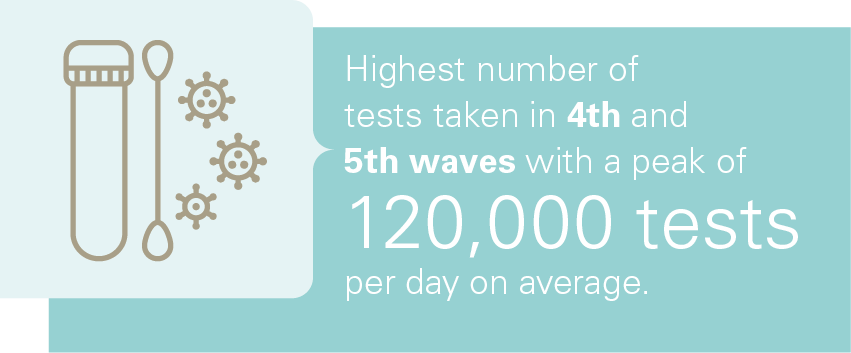
After the fifth wave, we observe a steep decline in the number of tests taken.
[1]Source: Sciensano.
[2]The positivity ratio represents the number of positive patients relative to the total number of people tested.
- Details
NUMBER OF COVID-19 PATIENTS IN GENERAL HOSPITALS
The number of hospital stays of COVID-19 patients was highest during the first and second wave. During the peaks of subsequent waves, half as many patients were admitted on average compared to the second wave in non-intensive care beds and one-third fewer patients in intensive care beds. Admissions to intensive care beds were significantly lower during the 5th wave. There are several factors that have had an impact on the number of hospitalisations: vaccination, more knowledge and experience in treatment among healthcare providers resulting in a shorter length of stay, a different mutation of the virus, better organisation of primary care, to name but a few.
NUMBER OF PATIENTS WITH COVID-19 INFECTION IN THE HOSPITAL[1]
BED OCCUPANCY RATES IN BEDS PROVIDED FOR COVID-19 PATIENTS IN
GENERAL HOSPITALS

The graphic below shows the occupancy rate of beds provided for COVID-19 patients for intensive and non-intensive care. During the peak of the first and second wave, the occupancy rates for both types of beds are similar, around 65% and 85% respectively. This changes in the third and fourth wave, where occupancy rates for intensive care beds are significantly higher, between 86% and 91%, than those for non-intensive care beds. In the fifth wave, we observe the opposite situation where the occupancy rate for non-intensive care beds with a peak of 83% is higher than that for intensive care beds (peak of 67%). This trend continues in the subsequent waves, with the peak in October 2022 reaching 71% for non-intensive care beds and 30% for intensive care beds.
BED OCCUPATION RATE EXPRESSED AS A PERCENTAGE OF THE TOTAL NUMBER OF BEDS PROVIDED [2]
The graphics below show the number of available intensive care and non-intensive care beds for COVID-19 patients as well as the number of COVID-19 patients who were admitted to the hospital. Here, we can clearly see that significantly more beds were reserved for COVID-19 patients during the first two waves than in the subsequent waves. To better understand these figures, it is important to take into account that a distribution plan was drawn up by the federal government that defines a system of redeploying beds (see chapter Organisation). This model informed hospitals of the number of beds they needed to make available for COVID-19 patients given the situation at the time. During the first wave, this model was not yet available. All non-essential care was shut down and the remaining beds were reserved for COVID-19 patients. This explains the lower occupancy rate during this period. This concerns the early period of the pandemic during which there was little knowledge and experience regarding the COVID-19 virus. At this time, the virus hit our country and surrounding countries hard. During the subsequent waves, an attempt was made to strike a balance between performing regular care and being able to accommodate the influx of COVID-19 patients. In addition, during the later waves, fewer beds were available because of staff absences due to constant, high workloads and infections, among other things.
NUMBER OF BEDS PROVIDED FOR COVID-19 PATIENTS IN NON-INTENSIVE CARE BEDS
NUMBER OF BEDS PROVIDED FOR COVID-19 PATIENTS
IN INTENSIVE CARE BEDS
PROFILE OF COVID-19 PATIENTS[3]
In 2020, 1.2% of all stays (i.e. classic hospitalisation, day hospitalisation and outpatient contacts with the emergency department) were COVID-19 patients.
NUMBER OF STAYS OF PATIENTS WITH AND WITHOUT A COVID-19 INFECTION IN 2020
Gender and age
When comparing characteristics of stays of COVID-19 patients with stays of non-COVID-19 patients in 2020 and stays in the period from 2016 to 2019, one finds that the number of hospitalised men and women is similar.
Furthermore, 79.9% of patients hospitalised with COVID-19 infection in 2020 was aged 50 or over. This is in sharp contrast with the age of patients without COVID-19 infection in 2020 (52.0%) and with the age of patients in the period from 2016 to 2019 (49.5%).
In the age groups from 40 to 79 years, in 2020 consistently more men with COVID-19 infection than women were hospitalised. We also find that more women than men were hospitalised in the age group from 20 to 39 years as well as in the age group from 80 years old. The higher number of women in the first group may in part be explained by the fact that this is the age at which women usually become pregnant. In that case, mild COVID-19 infection may have been detected when the woman was admitted to give birth[4]. It is also possible that these women were admitted out of precaution in the event of COVID-19 infection during pregnancy. In the second age group, from 80 years old, the higher number of hospitalised women can be explained by the fact that the female population is more numerous in this age group.
NUMBER OF STAYS OF COVID-19 PATIENTS BY SEX AND AGE GROUP IN 2020
Length of stay
The median[5]length of stay increases with the patient’s age, from 2 days for 0 to 9-year-olds to 12 days for people aged 80 and over.
MEDIAN OF LENGTH OF STAY BY AGE GROUP
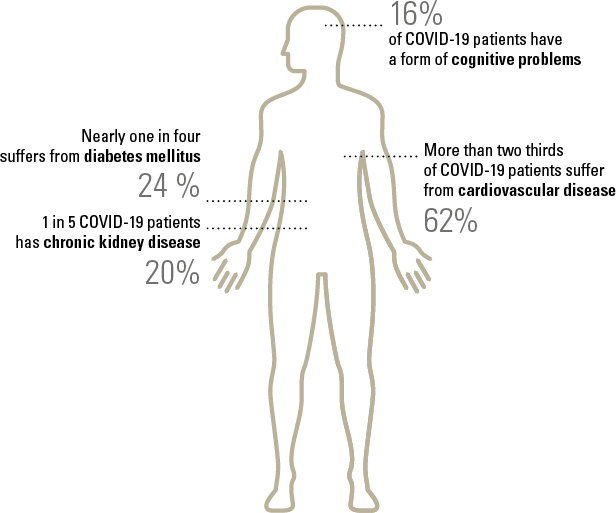
Comorbidity
Mortality in general hospitals
17% of all patients diagnosed with COVID-19 infection died in a hospital in 2020.
The percentage of deaths is higher for patients from assisted living facilities who were admitted to a hospital (35.9% compared to 14.5%).
PERCENTAGE OF DEATHS IN THE HOSPITAL ACCORDING TO WHETHER THE PATIENT STAYED IN AN ASSISTED LIVING FACILITY PRIOR TO THE HOSPITAL STAY
PROFILE OF COVID-19 PATIENTS IN INTENSIVE CARE
In 2020, 17.1% of patients with COVID-19 infection that were hospitalised were admitted in intensive care units.
NUMBER OF STAYS OF COVID-19 PATIENTS IN (NON-)INTENSIVE CARE
Gender and age
64.5% of all patients with COVID-19 infection who were admitted in intensive care units were male.
PERCENTAGE OF (NON)-INTENSIVE CARE STAYS BY SEX AMONG COVID-19 PATIENTS
| Intensive care | Non-intensive care |
85% of all stays of patients with COVID-19 infection in an intensive care unit pertained to patients between the ages of 50 and 89 in 2020.
NUMBER OF INTENSIVE CARE STAYS
BY AGE GROUP AMONG COVID-19 PATIENTS
Length of stay
|
MEDIAN OF LENGTH OF STAY |
The median of the total length of stay in hospital in 2020 was 15 days if the COVID-19 patient was admitted in an intensive care unit. For patients who were hospitalised in a regular nursing unit, the median of the length of stay was one week. |
Mortality in general hospitals
One third of COVID-19 patients admitted in an intensive care unit died in hospital in 2020. COVID-19 patients who did not end up in an intensive care unit died in 13.7% of cases.
PERCENTAGE OF DEATHS AMONG COVID-19 PATIENTS IN (NON-)INTENSIVE CARE
[1]Source: Sciensano
[2]Source: Sciensano and ICMS
[3]Source: Minimal hospital data (MHD), Data and Policy Information Service, FPS HSFCE. At the time of publication, our services only have data for 2020 to construct a profile of COVID-19 patients. All patients with confirmed or suspected COVID-19 infection were included in the figures, regardless of the reason for admission. It is also possible that patients who were transferred to a different hospital during their hospital stay were counted twice.
[4]It is impossible to determine whether the person was hospitalised due to COVID-19 infection or due to another condition, where COVID-19 infection was only detected by the mandatory test on admission.
[5]We have opted for showing the median value because this statistic is less affected by extreme values than the average. The median is the value situated exactly in the middle of a data set when you place the values from low to high. It is a centre value that separates the lowest 50% of the values from the highest 50%.
- Details
The first and second wave saw an average of over 200 deaths per day occurred within and outside of hospitals. This rate dropped significantly during subsequent waves, where the average number of daily deaths hovered around 50 deaths in the fourth and fifth wave. Since May 2022, the average has fluctuated between 4 to 14 deaths per day.
DAILY NUMBER OF DEATHS RESULTING FROM A COVID-19 INFECTION[1]
[1]Source: Sciensano
- Details
The vaccination campaign was divided into different phases:
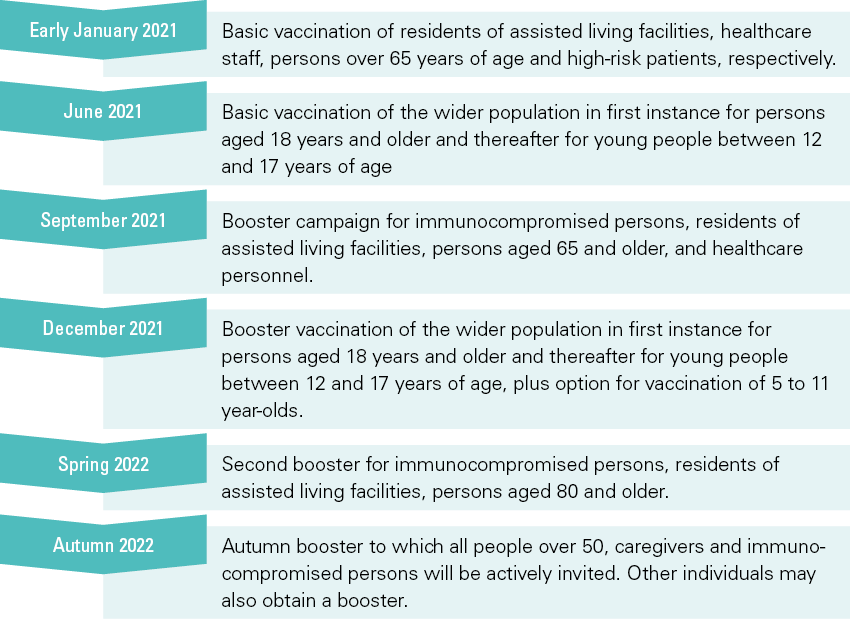
The graphic below gathers data from all persons who received a vaccine. By 31 October 2022, 79% of the total Belgian population had been given a basic vaccination. In addition, 62% had also been given a first booster vaccine, 31% a second booster vaccine and 4% an autumn booster.
PERCENTAGE OF VACCINATED PERSONS BY TYPE OF VACCINATION[1]
Below, we compare the percentage of vaccinated persons aged 18 years and older and the percentage of vaccinated healthcare workers by 31/10/2022. Here, we observe that the percentage of persons who received a complete baseline vaccination is similar. However, we notice a greater variation in the percentage of individuals who obtained a first and second booster. We see that a larger percentage of caregivers obtained a booster. Since the autumn booster, however, we see the first time that the general population was more likely to obtain the booster than caregivers, but this figure may still rise.
VACCINATION RATE AMONG CARE GIVERS
AND PERSONS AGED 18 AND OVER (31/10/2022)
[1]Source: Sciensano