The COVID-19 pandemic has had a major impact on the financial situation of hospitals and healthcare providers. The hospitals needed to implement emergency plans at short notice. Both increasing the admission capacity and increasing the capacity of the intensive care unit resulted in considerable additional costs.
In addition, non-essential care was postponed on several occasions, resulting in less revenue for the hospital and the healthcare providers through fee for service payment and fixed fees.

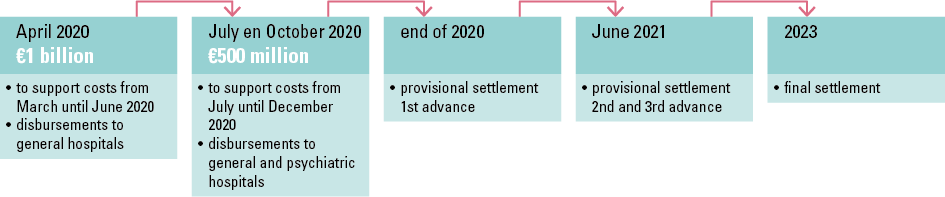
For this reason, the federal government decided in 2020 to provide financial compensation for hospitals and healthcare providers. To this end, advances totalling €2 billion were disbursed to general and psychiatric hospitals.
The aim of granting the advances was to support the hospitals in meeting their financial obligations, i.e. paying active staff members as well as paying invoices from suppliers and service providers on time.
|
The lump-sum payments are intended to provide support with the following:
|
The final funding will be calculated in 2023 taking into account the actual impact of COVID-19 on each hospital, and will be calculated and paid out in a collaboration between the FPS HSFCE and the NIHDI.
TIMELINE OF HOSPITAL FUNDING
Find out more about the specific rules for the disbursement of funding: www.ejustice.just.fgov.be
A staff member working in a general or psychiatric hospital between 1 September and 30 November 2020 is entitled to a one-off incentive payment of €985 gross[1]. In addition, as compensation for the COVID-19 efforts made, care staff from the federal sector (including hospitals, district health centres and home nursing services) are also entitled to consumption vouchers worth €300 per person that can be used in the catering and events sector[2].
Find out more about federal support for hospitals: www.health.belgium.be
In order to continue to guarantee their optimal operation, hospitals were stimulated to keep the bed occupancy rate under control. Patients had to be optimally distributed across the various hospitals and their campuses. In addition, patients who no longer needed hospital care had to leave the hospital as soon as possible. Hospitals were entitled to compensation for the transportation of patients to achieve the above. In 2020 and 2021, hospitals recorded 21,106 and 21,363 trips, respectively. This includes both trips within and outside the hospitals, and the transportation of COVID-19 as well as non-COVID-19 patients. On average, a little over €2 million per year was paid out to compensate hospitals for the costs of this patient transportation. These amounts were paid out via the Financial Resources Budget.
[1]Source:https://www.health.belgium.be/sites/default/files/uploads/fields/fpshealth_theme_file/faq_prime_dencouragement_pour_le_personnel_hospitalier-5_janvier_2021.pdf
[2]Source:Royal Decree of 22/12/2020 laying down the funding and arrangements for introducing a solidarity bonus in the federal healthcare sectors
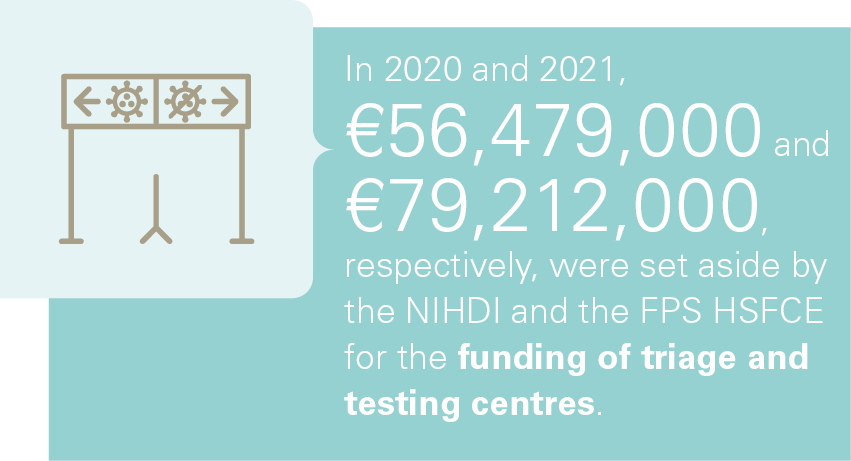
Funding is provided by the NIHDI and the federal government for both the start-up costs of the triage and testing centre and the medical costs, including medical coordination and compensation for doctors and nurses. Funding is also provided for administrative and support staff. In addition, a financial contribution for personal protective equipment was envisaged. The federated states contribute to the further operating costs of the centres[2].
[1]Source: NIHDI
[2]Source: Protocol Agreement concluded between the Federal Government and the authorities referred to in Articles 128, 130, 135 and 138 of the Constitution on the setting up, organisation and funding of triage and testing centres in the context of managing the COVID-19 crisis
The NIHDI provides a fixed fee for the services of doctors (coordination, follow-up, availability and direct care), nurses and healthcare assistants. The centres are paid on the basis of the number of hours worked. If care other than that of doctors and nurses is necessary, this will be organised through the regular channels. The patient’s insurance provider will receive information about their client’s stay in one of these centres.[1]

[1]Source: NIHDI
Protocol agreement on the reinforcement of mental healthcare
To respond to the increase in psychosocial problems associated with the COVID-19 pandemic, an extension of reimbursement for primary psychological care was approved. This way, in addition to adults, children, adolescents and over-65s are helped as well to consult a primary care provider for mild to moderate psychological problems.
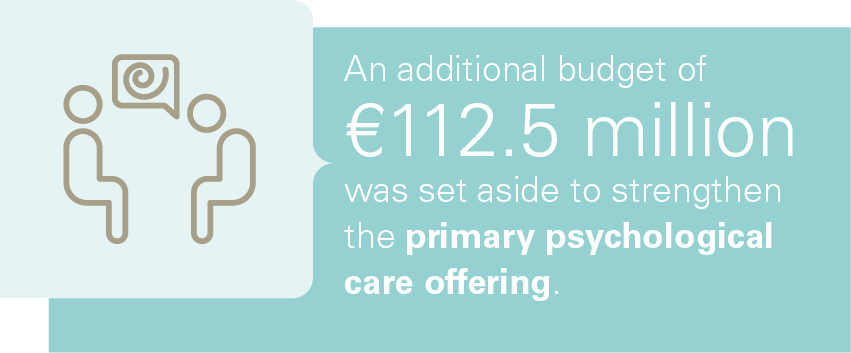
In addition, within the Interministerial Conference on Public Health (IMC), the competent Ministers concluded a protocol agreement on the coordinated approach to strengthening the provision of primary psychological care. The agreement sets out several priority target groups, including children and parents in vulnerable families, young adults and people with existing mental health problems. An additional budget of €112.5 million was set aside for this effort. This equates to a total of 1,986 full-time equivalent (FTE) psychological care providers.
Find out more about the protocol agreement: www.health.belgium.be
This new convention on primary psychological care completes the range of care actors by offering accessible and fast help to vulnerable groups with mild to moderate problems. Indeed, it is desirable to detect the need for psychological care as early as possible. The additional offer is aimed at children and adolescents as well as adults and elderly.
The aim of the convention is to bring about change in access to care.
- On the one hand, by facilitating financial access. To this end, two care functions will be financed within this framework:
-
- the primary psychological care function for support with mild to moderate problems
- the specialist psychological care function for support with moderate to severe problems
- On the other hand, by facilitating access to an accredited clinical psychologist or remedial educationalist by making them available in citizens’ immediate environment (i.e. focusing work on their natural environment). One wants to achieve that these care providers, in addition to the service provision in their practices, provide general care or even leisure activities at places where the vulnerable population goes for a purpose other than requesting psychological health support, e.g. an organisation for material or social assistance. This is motivated by the wish to offer assistance at a place that does not lead to stigmatisation. At a place that enables intersectoral and multidisciplinary collaboration with other care providers. These include, for instance, Public Social Welfare Centres, the Child and Family Agency, assistance in an open environment, homework schools, community centres, student guidance centres and GP practices.
In 2022, the various networks for mental healthcare have entered into new agreements with care providers based on a needs analysis of their area of activity within the framework of the protocol agreement. In the meantime, one can see that the number of people that have made use of the offer of primary psychological care is increasing.
Find out more about the agreement for the reimbursement of psychological care: www.riziv.fgov.be
Temporary measures during the pandemic
As the development of this convention takes time, a number of temporary measures aimed at vulnerable target groups have already been taken in this context. Indeed, various studies have shown that the mental well-being of adolescents and students, people living alone and professionals that are most affected by the pandemic (e.g. those working in healthcare, catering, the cultural sector) is under the greatest pressure.
In order to specifically meet the psychological needs of these most vulnerable groups, the following measures have been taken:
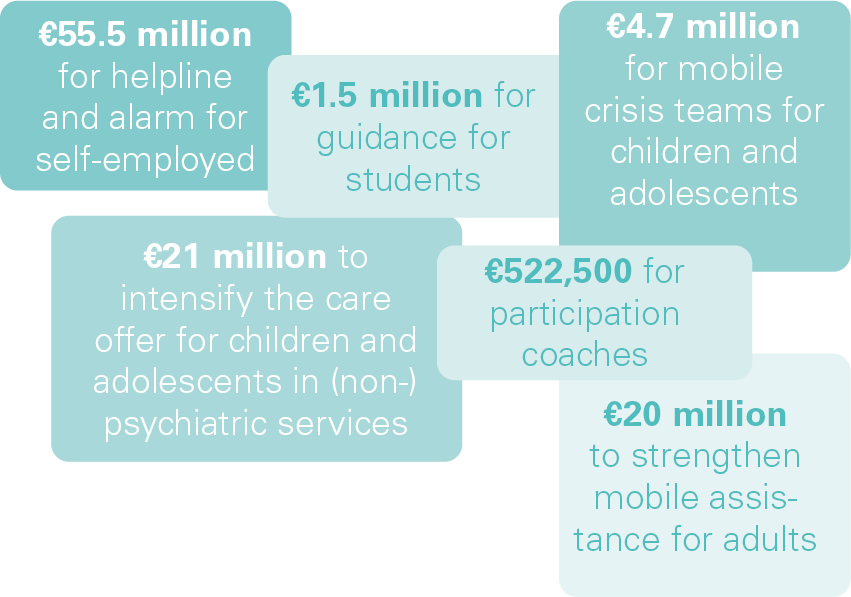
- Psychological care for self-employed with psychological needs through e.g. a free helpline and/or an alarm that is activated by explorers (e.g. trustees in bankruptcy, banks, business one stop shops, social insurance funds for self-employed, social secretariats and care providers) or clinical psychologists and remedial educationalists who regularly come into contact with self-employed persons. An annual budget of €55.5 million was set aside for this. This measure was in place until 28 February 2022.
- From 15 April 2021 to 31 December 2021, €1.5 million was set aside for guidance for students in colleges and universities. Group sessions with an emphasis on stress control and reinforcing the ability to cope were organised in order to prevent the development of psychological problems.
- Since February 2021, the measure was taken to provide faster assistance to children, adolescents and young adults with acute psychological problems or adolescents in a crisis situation by reinforcing the mobile crisis teams of the networks for mental healthcare for children and adolescents.
-
- the total budget for the mobile teams was increased by 50%;
- the operating resources for the networks by 75%;
- the resources for network psychiatrists by 25%.
This way, the capacity for mobile crisis assistance was expanded considerably in the short term through an additional budget of €4.7 million, which is the equivalent of approximately 50 FTE.
- In addition, it was decided in April 2021 to intensify the residential care offer for the assistance of children and adolescents with serious and complex psychological problems by increasing the personnel resources for psychiatric services for children and adolescents. Such intensification allows the personnel to take care of the transfer of care from the residential setting to the home or substitute home environment. The aim of this is to optimise the continuity of care for children and their families and reduce the length of stay in psychiatric services for children and adolescents. A total of 212 FTEs were financed. At the same time, it was also decided to increase the care capacity for assistance to children and adolescents with psychological problems in non-psychiatric hospital services by using so-called liaison teams from the psychiatric services for children and adolescents to e.g. paediatric services. A total of 23 teams of 2.70 FTEs each were financed. An additional annual budget of just over €21 million was set aside for these measures.
- In addition, participation coaches were added to the networks for mental healthcare for children and adolescents to increase the participation of adolescents and their environment in the development of their own care pathways and in policy at the level of the institution, the network and the government. An annual budget of €522,500 was set aside for this.
- It was also decided to reinforce the mobile assistance of the networks for mental healthcare for adults by 25% for the elderly target group. In doing so, the aim is to pay special attention to the socially and economically vulnerable and to those who tend to avoid care. To this end, mobile, outreaching and multidisciplinary care will be provided. An annual amount of more than €20 million was set aside for this, which allows to increase the mobile teams by 244 FTEs.
The latter 4 measures currently continue unabated.
Furthermore, numerous other actions were taken during the pandemic to strengthen mental healthcare provision, including:
- Reimbursement of video consultations by psychiatrists;
- Remote aftercare following admission to a psychiatric hospital[1];
- Possibility of partial hospitalisation at the patient’s home[2];
- Awareness-raising among primary healthcare professionals to encourage the safe use of psychopharmaceuticals;
- Training of hospital staff to improve the care of individuals with alcohol problems;
- Psychological support for hospital staff;
- Furthermore, additional resources were granted to the Flemish Cross for their cooperation in the management of the health crisis, including for offering psychosocial support in the COVID-19 call centre intended for the general public.
Project calls
In the spring of 2022 a call was launched to the networks for mental healthcare for children and adolescents to design 6 new sites for the target groups children, adolescents and young adults. These networks can submit proposals for the reinforcement of assistance to children, adolescents and young adults within their area of activity. Around €35 million is being invested in this. It is hoped to be able to meet the most urgent needs in each province. Certain flexibility is permitted in order to invest the budget made available where it is most needed. Based on a needs analysis, a decision will be made on how exactly the additional resources, complementary to the local offer and initiatives already present, will be used.
Find out more about this call: www.health.belgium.be
Furthermore, a project call was launched to the networks for adults to submit project proposals on the ‘Intensification of residential care’, so that in each network at least 1 High Intensive Care service is developed. This call implements the decision of the coalition agreement of 30 September 2020 to deploy more staff in psychiatric care programmes than provided for in the current rules for staff. An investment of €15 million has been planned for the deployment of an additional 150 staff and reinforcement with 193 hours of medical work.
More information: Working group on intensification of residential care
[1]Find out more about remote aftercare via NIHDI (fgov.be)
[2]Find out more about partial hospitalisation at home via NIHDI (fgov.be)
 |
In the context of tackling the pandemic, 22 ambulance services added an addendum to their agreement with the FPS HSFCE in 2020. On the basis of this addendum, a standard allowance of ± €12,000 was granted for a period of 8 weeks for each on-call unit within the ambulance service that was available 24/7. In addition, a one-off amount of €8 million was divided between the ambulance services in the context of the COVID-19 pandemic. |
